- What is GLP-1?
- How GLP-1 Drives Weight Loss?
- How GLP-1 Manages Diabetes?
- What are GLP-1 Agonists?
- List of GLP-1 agonists
- How GLP-1 Agonists Work Differently from GLP-1/Glucagon-like Peptide-1?
- Potential Benefits of GLP-1 Agonists
- Side Effects of GLP-1 Agonists
- Next Steps: Taking Action with GLP-1 Therapies
- Conclusion
GLP-1, or Glucagon-like Peptide-1, is transforming the way we approach metabolic health. Initially studied for its role in controlling blood sugar in type 2 diabetes, GLP-1 has now gained attention for its remarkable effects on weight management.
By naturally regulating appetite, enhancing insulin secretion, and slowing gastric emptying, this hormone and its synthetic agonists offer a dual benefit for those looking to manage both diabetes and weight.
This article explores how GLP-1 works in the body to drive these outcomes, the differences between natural GLP-1 and synthetic agonists, and how to effectively navigate treatment options for sustainable health.
What is GLP-1?
Glucagon-like peptide-1 (GLP-1) is a naturally occurring incretin hormone primarily produced by L-cells in the small intestine, playing a major role in regulating blood sugar levels, appetite, and overall metabolic health.
Released rapidly in response to nutrient ingestion, especially carbohydrates and fats, it enhances insulin secretion from pancreatic beta cells in a glucose-dependent manner, effectively lowering postprandial blood glucose without risking hypoglycemia.
How GLP-1 Drives Weight Loss?
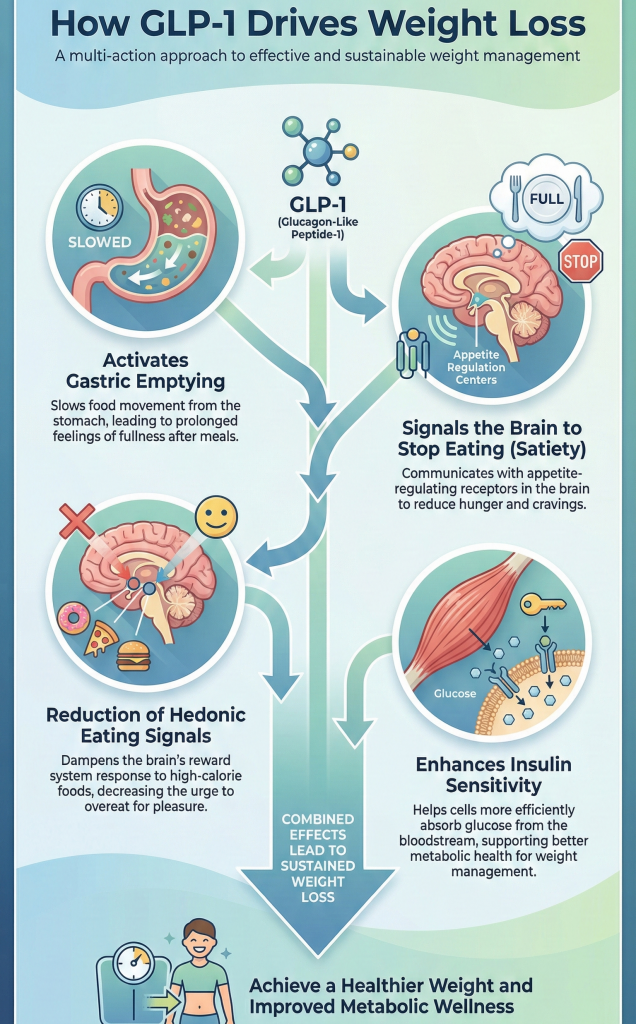
- Activates The Gastric Emptying:
When GLP-1 is released from the gut, it binds to receptors in the stomach muscles, slowing the movement of food from the stomach into the small intestine. As a result, food remains in the stomach longer, promoting an earlier and prolonged sensation of fullness after meals.
- Signals The Brain To Stop Eating (Satiety):
GLP-1 crosses the blood-brain barrier and interacts with appetite-regulating receptors in the hypothalamus. This generates a strong satiety signal, reducing hunger and cravings, and helping to curb the desire for unnecessary snacking.
- Reduction of Hedonic Eating Signals:
By acting on the brain’s reward centers, GLP-1 diminishes the pleasure response associated with high-calorie foods. This decreases intrusive thoughts about eating, making it easier to adhere to smaller portion sizes without feeling deprived.
- Enhances Insulin Sensitivity:
GLP-1 improves insulin sensitivity, particularly in muscle tissue, allowing cells to utilize glucose more efficiently for energy rather than storing it as fat. While this metabolic effect supports weight management, the primary driver of GLP-1–mediated weight loss is reduced calorie intake rather than a substantial increase in energy expenditure.
How GLP-1 Manages Diabetes?
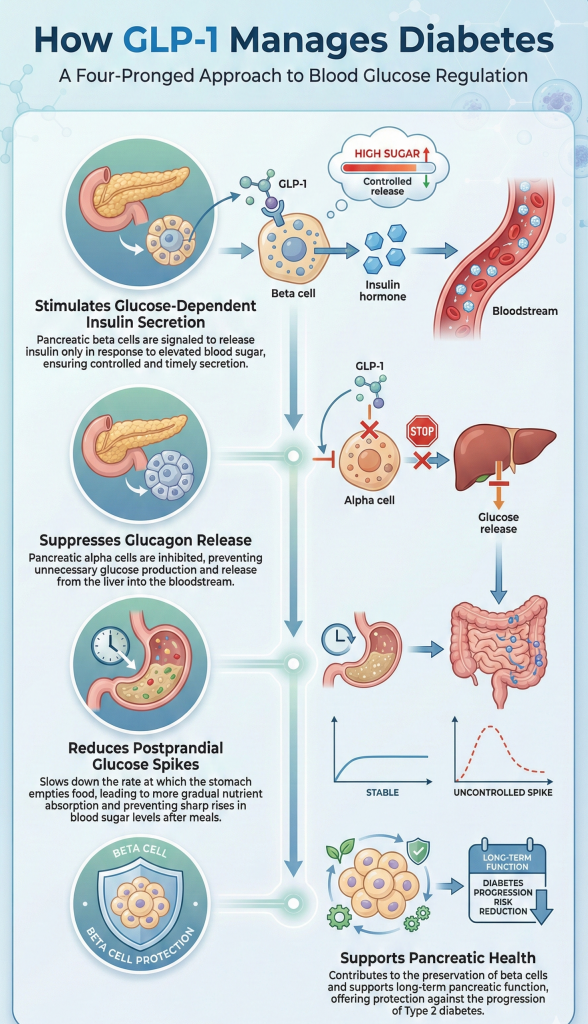
- Stimulates Glucose-Dependent Insulin Secretion:
GLP-1 acts on pancreatic beta cells to enhance insulin release in response to elevated blood glucose levels. This glucose-dependent mechanism ensures that insulin is secreted only when necessary, reducing the risk of hypoglycemia once blood sugar returns to normal.
- Suppresses Glucagon Release:
GLP-1 inhibits the secretion of glucagon from pancreatic alpha cells. Since glucagon signals the liver to release stored glucose into the bloodstream, its suppression prevents unnecessary sugar release, thereby helping to lower overall blood glucose levels.
- Reduces Postprandial Glucose Spikes:
By slowing gastric emptying, GLP-1 ensures that nutrients are absorbed gradually rather than rapidly. This mitigates sharp post-meal spikes in blood sugar, promoting more stable glucose levels throughout the day.
- Supports Pancreatic Health:
Over time, GLP-1 reduces stress on beta cells and promotes their survival, preserving the pancreas’s natural ability to produce insulin. In Type 2 diabetes, where beta cells often deteriorate, GLP-1 helps slow disease progression and maintain endogenous insulin production.
While GLP-1 plays a crucial role in managing diabetes, combining it with tailored nutritional strategies can further enhance metabolic stability and overall health.
Programs like The Certificate Program in Nutrition Strategies for Lifelong Health and Wellness from Duke University School of Medicine equip learners to integrate these insights into practical, evidence-based nutrition plans. The program helps you to:
- Gain Confidence With GLP-1 & Related Therapies: Understand GLP-1 mechanisms, indications, benefits, and risks to design nutrition plans that preserve lean mass and support overall treatment outcomes.
- Personalize Nutrition For Every Stage Of Life: Tailor dietary strategies from pregnancy to older adulthood to support healthy aging and address medical conditions.
- Master Gut Microbiome Nutrition: Create microbiome-informed diets that improve intestinal absorption and barrier function using prebiotics, probiotics, and fibers.
- Manage Chronic Diseases With Food: Apply “food-as-medicine” principles to tackle obesity, diabetes, and cardiometabolic risks.
- Navigate Diet Trends With Science: Critically evaluate popular diet myths and provide evidence-based guidance for lifelong healthy habits.
Certificate Program in Nutrition Strategies
Build a strong foundation in whole-food nutrition, metabolic health, and evidence-based dietary strategies to achieve lasting health and wellness transformations.
However, despite its potent effects, endogenous GLP-1 has a very short half-life of just 1-2 minutes due to rapid degradation by the dipeptidyl peptidase-4 (DPP-4) enzyme.
This limitation has driven the development of synthetic GLP-1 receptor agonists (GLP-1RAs). Let's understand that now
What are GLP-1 Agonists?
GLP-1 agonists (also known as GLP-1 receptor agonists or analogs) are a class of synthetic medications designed to mimic the actions of the natural GLP-1 hormone.
They bind to the same receptors in the pancreas and brain to lower blood sugar and suppress appetite.
However, unlike the natural hormone, which breaks down in minutes, agonists are chemically modified to resist degradation, allowing them to remain active in the body for hours or days to provide continuous metabolic control.
List of GLP-1 agonists
1. Semaglutide
Currently, the most prominent active ingredient in this class is available in both injectable and oral forms.
- Ozempic (Injection)
- Indication: Type 2 Diabetes, cardiovascular risk reduction
- Frequency: Weekly
- Wegovy (Injection)
- Indication: Chronic weight management (obesity or overweight with comorbidities)
- Frequency: Weekly
- Rybelsus (Tablet)
- Indication: Type 2 Diabetes.
- Frequency: Daily (oral)
2. Tirzepatide (Dual Agonist)
Technically a dual GIP/GLP-1 receptor agonist, this drug acts on both GLP-1 and GIP receptors for potentially higher efficacy.
- Mounjaro (Injection)
- Indication: Type 2 Diabetes
- Frequency: Weekly
- Zepbound (Injection)
- Indication: Chronic weight management
- Frequency: Weekly
3. Liraglutide
An older, daily formulation often used before weekly options became available.
- Victoza (Injection)
- Indication: Type 2 Diabetes, cardiovascular risk reduction
- Frequency: Daily
- Saxenda (Injection)
- Indication: Chronic weight management
- Frequency: Daily
4. Dulaglutide
- Trulicity (Injection)
- Indication: Type 2 Diabetes, cardiovascular risk reduction
- Frequency: Weekly
5. Exenatide
The first class of GLP-1s was approved; they are generally less commonly prescribed now due to newer, more convenient options.
- Byetta (Injection)
- Indication: Type 2 Diabetes
- Frequency: Twice daily
- Bydureon BCise (Injection)
- Indication: Type 2 Diabetes
- Frequency: Weekly (Extended-release)
6. Lixisenatide
- Adlyxin (Injection)
- Indication: Type 2 Diabetes.
- Frequency: Daily.
- Soliqua (Combination Injection)
- Contains: Lixisenatide + Insulin Glargine.
- Indication: Type 2 Diabetes.
Note: Tirzepatide is technically a dual agonist (GLP-1 + GIP), meaning it targets two hormone receptors for potentially stronger effects.
How GLP-1 Agonists Work Differently from GLP-1/Glucagon-like Peptide-1?
| Feature | Natural GLP-1 | GLP-1 Agonists | Result / Impact |
| Survival Time (Half-Life) | Rapidly degraded by DPP-4 within 1.5–2 minutes, acts as a brief, meal-dependent signal. | Chemically modified to resist DPP-4 degradation (“armored”), lasts 24 hours (Liraglutide) or 7 days (Semaglutide) | Provides constant, sustained receptor activation rather than fleeting control |
| Activation Pattern (Pulsatile vs. Continuous) | Works in pulses, spikes after meals, and drops during fasting, the body gets intermittent signaling | Continuous high-level activation, receptors in the brain and pancreas are stimulated 24/7, even without food intake. | Continuous receptor stimulation promotes significant satiety and more pronounced weight loss |
| Concentration Levels (Physiological vs. Pharmacological) | Produced in physiological (normal/low) amounts, sufficient to manage the food consumed | Administered at pharmacological (supraphysiological) doses that are several times higher than natural GLP-1 | Enables stronger biological effects, including slowed gastric emptying and sustained appetite suppression |
Potential Benefits of GLP-1 Agonists
- Lowering Blood Pressure: Reduces elevated blood pressure, supporting cardiovascular health.
- Improving Lipid Disorders: Normalizes cholesterol and triglyceride levels, enhancing metabolic function.
- Improving Fatty Liver Disease: Reduces fat accumulation in the liver, improving liver function.
- Reducing Risk of Heart and Kidney Disease: Lowers the likelihood of cardiovascular and renal complications.
- Delaying Progression of Diabetes-Related Nephropathy: Slows kidney damage associated with chronic diabetes.
Side Effects of GLP-1 Agonists
Common side effects may include
- Nausea
- Vomiting
- Diarrhea
- Loss of Appetite
This occurs especially when starting the medication or increasing the dose. Other mild effects can be:
- Dizziness,
- Headache
- Upset Stomach
- Temporary Redness At The Injection Site
Severe side effects are rare but may include pancreatitis, thyroid cancer, kidney injury, or worsening eye complications related to diabetes.
Next Steps: Taking Action with GLP-1 Therapies
- Consult a Healthcare Professional: Discuss your eligibility for GLP-1 agonists with a doctor or endocrinologist. They can assess your medical history, current medications, and potential risks.
- Set Realistic Goals: Establish achievable targets for weight loss and blood sugar control. GLP-1 therapies work best when combined with lifestyle modifications.
- Adopt a Balanced Diet: Focus on nutrient-dense foods and controlled portions. GLP-1 enhances satiety, making it easier to adhere to a healthy eating plan.
- Incorporate Regular Exercise: Physical activity complements GLP-1 effects by improving insulin sensitivity, promoting cardiovascular health, and supporting weight management.
- Monitor Progress: Track your health care analytics, such as blood glucose levels, weight, and overall well-being regularly. Adjustments to dosage or lifestyle may be required based on results.
By taking these steps, individuals can maximize the benefits of GLP-1–based treatments and achieve sustained improvements in both metabolic health and quality of life.
Conclusion
With the people struggling to manage weight and type 2 diabetes, GLP-1 and GLP-1 agonists offer an effective solution. While natural GLP-1 regulates blood sugar and appetite, GLP-1 agonists enhance and extend these effects, supporting better glucose control, reduced hunger, and sustainable weight management.