Overwhelmed by the abundance of fad diets and inconsistent nutrition advice, many individuals find it difficult to identify what truly supports long-term health.
This is where the Dietary Reference Intakes (DRIs) come in. It provides scientifically backed guidelines on the nutrients your body needs, the recommended amounts, and the frequency for optimal health.
In this blog, we will break down what DRIs are, which foods help meet these requirements, and how to create a diet plan using dietary reference intakes.
What are Dietary Reference Intakes (DRIs)?
Dietary Reference Intakes (DRIs) are a set of scientifically established guidelines that define the recommended nutrient intakes for healthy individuals. They are designed to:
- Prevent Deficiencies
- Reduce The Risk Of Chronic Diseases
- Promote Overall Health
DRIs provide benchmarks for essential nutrients, including vitamins, minerals, proteins, fats, and carbohydrates, tailored to different age groups, genders, and life stages.
Key Components of DRIs
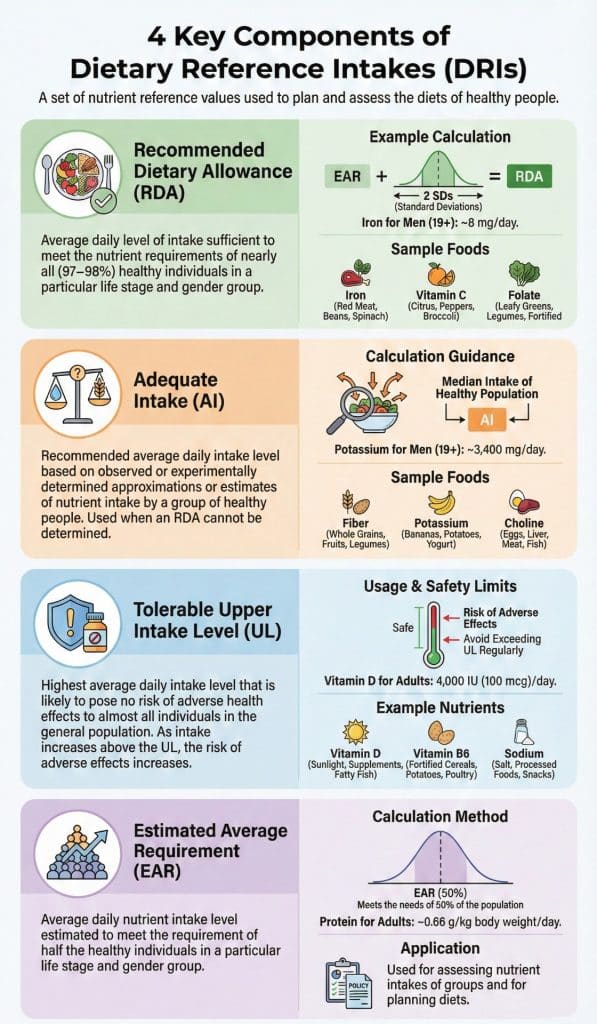
1. Recommended Dietary Allowance (RDA)
The average daily dietary nutrient intake level is sufficient to meet the nutrient requirements of nearly all (97–98%) healthy individuals in a particular life stage and gender group.
Calculation: It is derived mathematically from the Estimated Average Requirement (EAR). The formula typically adds two standard deviations (SD) to the EAR to ensure coverage for the vast majority of the population.
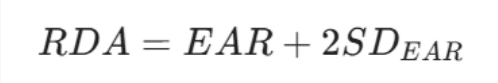
(If the Standard Deviation is unknown, a Coefficient of Variation of 10% is usually assumed, making the calculation: RDA = 1.2 X EAR)
Usage:
- For Individuals: This is the "gold standard" target. Dietitians use the RDA to set daily goals for clients to ensure they are not deficient.
- Diet Planning: Menus for schools or hospitals are often planned to meet the RDA to ensure nutritional adequacy for almost everyone.
2. Adequate Intake (AI)
An average daily nutrient intake based on observations or experiments in healthy individuals, used when an RDA cannot be determined.
Calculation: Unlike the RDA, the AI is not calculated from the EAR. Instead, it relies on:
- Observation: The median intake of a healthy population (e.g., what healthy breastfed infants naturally consume).
- Expert Judgment: Estimates derived when scientific evidence is insufficient to calculate a precise statistical requirement.
Usage:
- For Individuals: Used as a goal when no RDA exists. It implies "we are sure this amount is healthy, but we don't have enough data to be statistically precise."
- Infant Nutrition: Almost all nutrient recommendations for infants (0–6 months) are AIs (based on breast milk composition).
3. Tolerable Upper Intake Level (UL)
The highest average daily nutrient intake level that is likely to pose no risk of adverse health effects to almost all individuals in the general population. As intake exceeds the UL, the potential for adverse effects may increase.
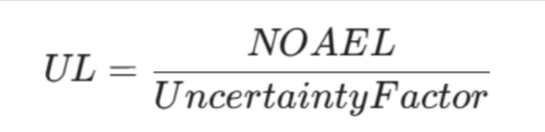
Calculation:
It is based on the No Observed Adverse Effect Level (NOAEL), the highest dose shown not to cause harm in studies, multiplied by an Uncertainty Factor (UF) to add a safety buffer.
Usage:
- Safety Ceiling: Crucial for people taking supplements or eating fortified foods. It is not a goal to reach, but a limit to avoid.
- Labeling: Helps regulators set limits on how much of a nutrient can be added to energy drinks or vitamins.
Risk: Exceeding the dosage can cause gastrointestinal distress, nausea, and constipation. This is rarely reached by food alone but easily reached with high-dose supplements.
4. Estimated Average Requirement (EAR)
A nutrient intake value that is estimated to meet the requirement of half (50%) of the healthy individuals in a life stage and gender group.
Calculation: determined by reviewing scientific literature to find the median point of requirement. It represents the 50th percentile of nutritional need.
Usage:
- For Populations: Used by policymakers to assess the nutrient adequacy of large groups (e.g., "What percentage of the US population is deficient in Vitamin D?").
- Scientific Baseline: The foundation used to calculate the RDA. It should NOT be used as a goal for individuals, because meeting the EAR means there is a 50% chance the individual is still deficient.
Step-By-Step: How To Create A Diet Plan Using Dietary Reference Intakes
To create a diet plan using Dietary Reference Intakes (DRI), you must move beyond simple calorie counting to ensure you meet specific nutrient requirements (macros and micros) set by scientific standards.
Let's understand this with a real example.
Example of The Adult Maintenance
- Name: Sarah
- Age: 30 years old
- Sex: Female
- Weight: 65 kg (143 lbs)
- Height: 165 cm (5'5")
- Activity Level: Moderately Active (exercises 3–4 times/week)
- Goal: Maintain current weight and improve energy.
Step 1: Determine Energy Needs (EER)
First, we calculate the Estimated Energy Requirement (EER). This tells us how many calories Sarah needs to maintain her weight. We use the Mifflin-St Jeor equation, which is standard for this purpose.
1. Calculate Basal Metabolic Rate (BMR):
BMR = (10 X weight) + (6.25 X height) - (5 X age) - 161
- 10 X 65 = 650
- 6.25 X 165 = 1,031 (approx)
- 5 X 30 = 150
- 650 + 1,031 - 150 - 161 =1,370 kcal/day (Calories burned at rest)
2. Apply Activity Factor:
For "Moderately Active," the DRI standard multiplier is roughly 1.55.
1,370 X 1.55 = 2,123.5 kcal/day
Target: Sarah needs - 2,123.5 calories daily.
Step 2: Set Macronutrient Ranges (AMDR)
Next, we distribute those calories using the DRI's Acceptable Macronutrient Distribution Ranges (AMDR). This ensures she gets enough fuel and building blocks for her body.
| Macronutrient | DRI Range (Adults) | Sarah's Selection | Math (based on 2,125 kcal) | Grams Needed |
| Carbohydrates | 45–65% | 50% (Moderate) | 2,125 X 0.50 = 1,062 kcal | 1,062 / 4 = 265g |
| Protein | 10–35% | 20% (Sufficient) | 2,125 X 0.20 = 425 kcal | 425 / 4 =106g |
| Fats | 20–35% | 30% (Healthy) | 2,125 X 0.30 = 638 kcal | 638 / 9 =71g |
(Note: Carbs & Protein = 4 kcal/g, Fat = 9 kcal/g)
Step 3: Identify Key Micronutrients (RDA/AI)
We must check the RDA (Recommended Dietary Allowance) for her specific age/sex group (Female, 19–50). We will focus on three "at-risk" nutrients for this demographic.
- Iron: RDA is 18 mg/day. (Vital due to menstruation; strictly plant-based eaters need 1.8x more).
- Calcium: RDA is 1,000 mg/day. (Vital for bone density).
- Fiber: AI (Adequate Intake) is 25 g/day (or 14g per 1,000 kcal).
Step 4: Create the Menu
Now, we select foods that fit the macro budget (Step 2) while hitting the micro targets (Step 3).
Breakfast: Calcium Focus
- Food: 1 cup Oatmeal made with 1 cup Low-fat Milk (or fortified Soy milk).
- Add-ons: 1 Banana + 1 tbsp Chia Seeds.
- Why: Milk provides ~300mg Calcium (30% of RDA); Chia seeds add Fiber and healthy Fats.
Lunch: Iron Focus
- Food: Spinach Salad (2 cups) with Grilled Chicken Breast (150g) and Chickpeas (1/2 cup).
- Dressing: Olive oil vinaigrette.
- Side: 1 Orange.
- Why: Spinach and Chickpeas provide Iron. The Vitamin C in the orange triples the iron absorption from the greens.
Snack: Protein Bridge
- Food: Greek Yogurt (150g) + 20 Almonds.
- Why: High protein helps satiety; almonds provide healthy fats and Magnesium.
Dinner: Omega-3 & Fiber
- Food: Baked Salmon (150g).
- Side: 1 cup Quinoa + 1 cup Roasted Broccoli.
- Why: Salmon hits the protein goal. Quinoa is a high-fiber carb source. Broccoli adds extra Calcium and Fiber.
Step 5: Review Against DRI
Let's see if Sarah's day met the scientific standards.
| Nutrient | Sarah's Goal (DRI) | Menu Estimated Total | Status |
| Calories | ~2,125 | ~2,100 | ✅ On Target |
| Protein | 106g | ~115g | ✅ Good (Slightly over is safe) |
| Fiber | 25g | ~32g | ✅ Excellent (Heart health) |
| Iron | 18mg | ~19mg | ✅ Met (Thanks to spinach/chickpeas) |
| Calcium | 1,000mg | ~1,100mg | ✅ Met (Thanks to milk/yogurt/broccoli) |
Sarah's case illustrates that effective diet planning goes beyond counting calories, requiring a deep understanding of nutrient science to separate breakthrough discoveries from fleeting trends, and programs like the Certificate Program in Nutrition Strategies for Lifelong Health and Wellness from Duke University School of Medicine offer a 9-week online curriculum designed to teach these evidence-based frameworks.
Certificate Program in Nutrition Strategies
Build a strong foundation in whole-food nutrition, metabolic health, and evidence-based dietary strategies to achieve lasting health and wellness transformations.
The program covers skills directly applied in Sarah’s example, with Module 1 focusing on Foundations of Nutrient Science and Energy Balance, as well as Micronutrients, DRIs, and their impact on menu planning.
Led by Duke faculty and industry experts, the program equips participants with practical tools and research-backed strategies to design personalized nutrition plans and translate complex science into meaningful, measurable outcomes, whether for personal use or professional practice.
Example 2- The Pregnant Lady
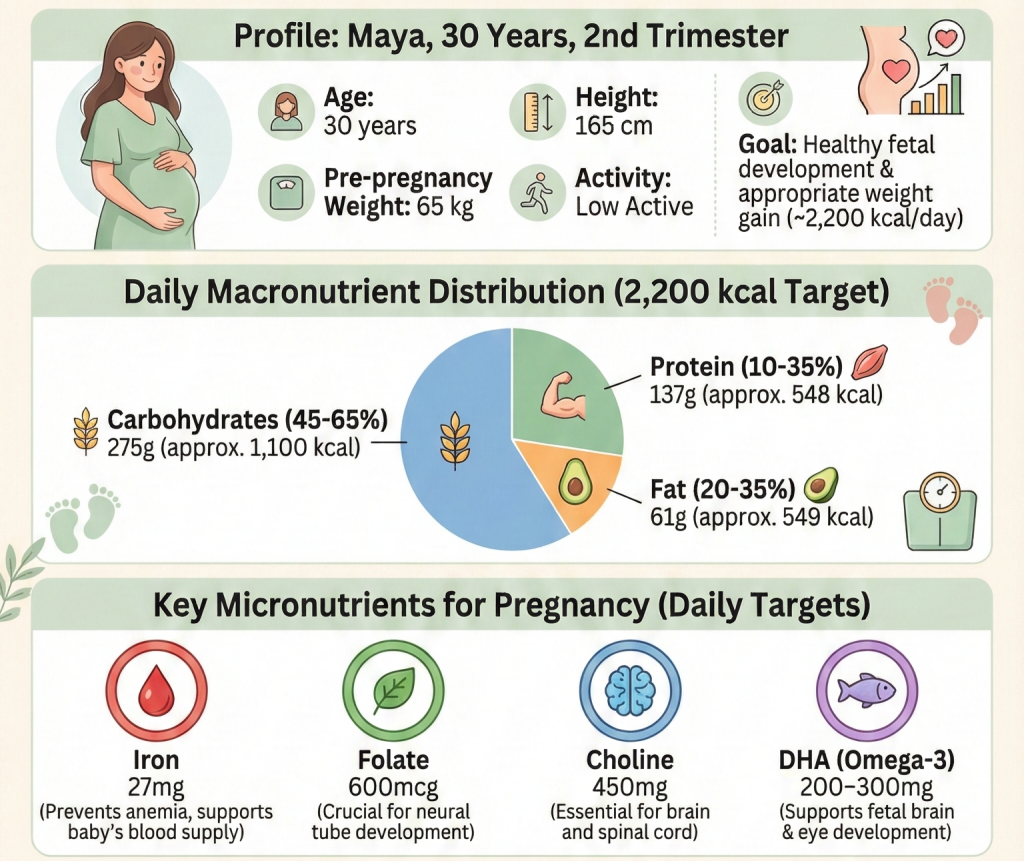
Designing a diet plan for pregnancy requires careful attention to Dietary Reference Intakes (DRIs), as the body's demands change significantly to support fetal growth. The focus shifts from just "maintenance" to nutrient density (specifically Iron, Folate, and Choline).
- Name: Maya
- Status: Pregnant (2nd Trimester)
- Age: 30 years old
- Pre-pregnancy Weight: 65 kg (143 lbs)
- Height: 165 cm (5'5")
- Activity Level: Low Active (Light walking/Yoga)
- Goal: Healthy fetal development and appropriate weight gain.
Step 1: Determine Energy Needs (EER + Pregnancy Increment)
Energy needs during pregnancy are calculated by adding a "pregnancy cost" to the woman's non-pregnant needs, based on the trimester. We will use the same Mifflin-St Jeor baseline as before, but with a slightly lower activity factor (typical of pregnancy fatigue).
- BMR: -1,370 kcal/day (Calculated based on pre-pregnancy weight).
- Activity (Low Active): Factor is 1.35.
- 1,370 X 1.35 = 1,850 kcal/day (Approx).
Add Pregnancy Increment: The DRI standards for energy addition are:
- 1st Trimester: +0 kcal
- 2nd Trimester: +340 kcal
- 3rd Trimester: +452 kcal
- 1,850 + 340 = 2,190 kcal/day
Target: Maya needs -2,200 calories daily.
Step 2: Set Macronutrient Ranges (AMDR)
The distribution changes slightly. Protein needs increase to support tissue synthesis, and carbohydrates are crucial for the baby's glucose needs.
| Macronutrient | DRI Range (Pregnancy) | Maya's Selection | Math (based on 2,200 kcal) | Grams Needed |
| Carbohydrates | 45–65% | 50% | 2,200 X 0.50 = 1,100 kcal | 1,100 / 4 =275g |
| Protein | 10–35% | 25% (High Priority) | 2,200 X 0.25 = 550 kcal | 550 / 4 = 137g |
| Fats | 20–35% | 25% | 2,200 X 0.25 = 550 kcal | 550 / 9 =61g |
Note: The absolute minimum RDA for carbs during pregnancy rises to 175g/day to ensure the fetal brain has enough glucose.
Step 3: Identify Key Micronutrients (RDA)
Pregnancy DRIs have specific spikes for "Critical Periods" of development. So, the nutrients below will be beneficial:
- Iron: RDA jumps from 18mg to 27 mg/day. (Needed for the expanded blood volume. This is very hard to hit with food alone, so we can include supplements.
- Folate (Vitamin B9): RDA is 600 mcg DFE. (Crucial for preventing neural tube defects).
- Choline: AI (Adequate Intake) is 450 mg/day. (Vital for fetal brain and memory development).
- Omega-3 (DHA): Not a strict RDA, but highly recommended (200-300mg) for eye/brain development.
Step 4: Create the Menu (Nutrient Dense)
We need foods that provide higher calories and these specific micros.
Breakfast: Folate & Iron Booster
- Food: 1 cup Fortified Breakfast Cereal (Check label for 50-100% Iron/Folate).
- Fluid: 1 glass of orange juice (Vitamin C helps absorb the non-heme iron from the cereal).
- Why: Fortified grains are the easiest way to hit the high Iron/Folate target.
Lunch: Protein & Fiber
- Food: Lentil & Spinach Soup (1.5 cups) with a whole wheat roll.
- Add-on: 3 oz Grilled Chicken Breast (chopped into soup).
- Why: Lentils are rich in Folate (approx 350mcg per cup) and Fiber. Chicken provides the extra protein needed for tissue growth.
Snack: The "Brain Builder" (Choline)
- Food: 2 Hard-Boiled Eggs + Apple slices.
- Why: Egg yolks are one of the richest sources of Choline (approx 150mg per egg). This snack hits 60% of the Choline goal.
Dinner: DHA (Omega-3)
- Food: Baked Salmon (fully cooked, 150g).
- Side: Sweet Potato (Vitamin A) + Green Beans.
- Why: Salmon provides the DHA needed for the baby's brain. Sweet potatoes offer safe Vitamin A (Beta-carotene).
Step 5: Review Against DRI
Did Maya meet the elevated pregnancy requirements?
| Nutrient | Maya's Goal (Pregnant) | Menu Estimated Total | Status |
| Calories | ~2,200 | ~2,150 | ✅ Good Range |
| Protein | 71g (Min) - 137g (Goal) | ~140g | ✅ Excellent for growth |
| Iron | 27mg | ~22mg | Needs Supplement For Complete Range |
| Folate | 600mcg | ~700mcg | ✅ Met (Thanks to lentils/cereal) |
| Choline | 450mg | ~480mg | ✅ Met (Thanks to eggs) |
Even with a perfect diet, hitting 27mg of Iron is difficult without over-consuming calories. This is why prenatal vitamins are a standard recommendation to bridge that specific DRI gap.
Importance of DRIs in Medicinal Nutrition
Medical Nutrition Therapy (MNT) uses Dietary Reference Intakes (DRIs) as a foundational guideline and adapts them to manage a wide range of medical conditions, including:
- Wound Healing
- Diabetes
- Renal Disorders
- Cardiovascular Disease
- Gastrointestinal Disorders
- Other Critical Illness
In situations such as wound healing after surgery, burns, or pressure ulcers, the body enters a hypermetabolic state characterized by increased energy expenditure and accelerated protein breakdown to support tissue repair. Patients with extensive wounds are therefore at a higher risk of:
- Malnutrition
- Delayed Healing
- Increased Susceptibility To Infection
In such cases, DRIs guide healthcare professionals in tailoring dietary intake to meet the elevated nutrient and energy requirements, thereby promoting optimal recovery and overall health.
To better understand this concept, consider the example of an individual recovering from major abdominal surgery with a large incision representing a stage 3 healing demand.
Example of Rapid Repair & Recovery Protocol
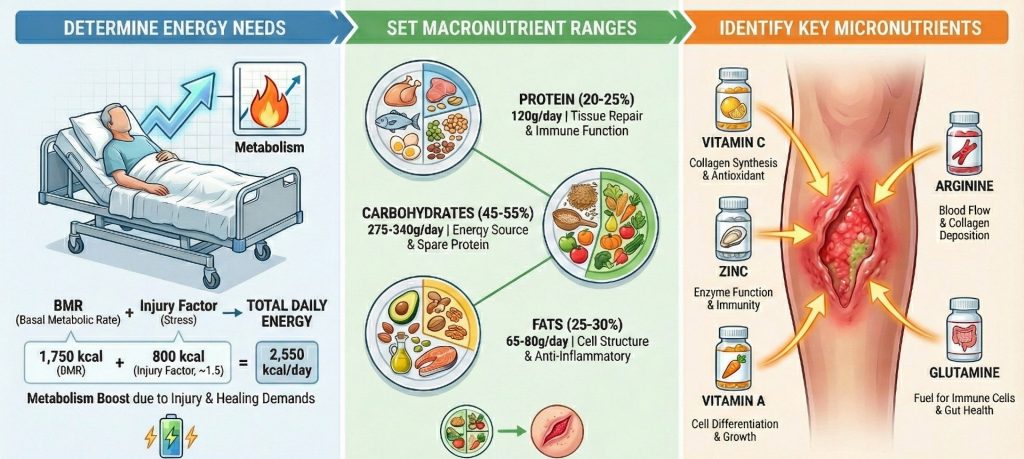
- Name: John
- Age: 55 years old
- Weight: 80 kg (176 lbs)
- Height: 180 cm (5'11")
- Activity Level: Bed rest / Low movement.
- Goal: Rapid tissue regeneration and infection prevention.
Step 1: Determine Energy Needs (EER + Injury Factor)
John needs calories to fight the "stress response" of injury. We use an Injury Factor (IF) rather than just an activity factor.
Calculate Basal Metabolic Rate (BMR):
- Using Mifflin-St Jeor for an 80kg male: ~1,750 kcal/day.
Apply Injury/Stress Factor:
- For major surgery/wound healing, the factor is typically 1.3 to 1.5.
- 1,750 X1.4 (average stress) = 2,450 kcal/day.
Alternatively, a quick medical shorthand is 30–35 kcal/kg: 80 kg X 30 = 2,400 kcal.
- Target: John needs ~2,450 calories (despite being in bed, his metabolism is racing to heal).
Step 2: Set Macronutrient Ranges
Standard DRI for protein is 0.8 g/kg. For wound healing, this nearly doubles to 1.5 g/kg because the body is synthesizing collagen and new skin cells rapidly.
| Macronutrient | Standard DRI | Wound Healing Goal | Math (for 80kg John) | Grams Needed |
| Protein | 0.8 g/kg | 1.5 g/kg | 80kg X 1.5 | 120g (High Priority) |
| Carbohydrates | 45–65% | 50% | Fuel for leukocytes (white blood cells) | 306g |
| Fats | 20–35% | 30% | Cell membrane integrity | 81g |
Step 3: Identify Key Micronutrients (Therapeutic Dosing)
Here is where MNT deviates from standard DRIs. We use Therapeutic Doses, which are often 10–50 times the RDA to saturate tissues at the wound site.
Vitamin C: Essential for collagen cross-linking (strength of the new skin).
- Standard RDA: 90 mg.
- Wound Therapy: 500mg – 1,000mg daily. (Requires supplementation).
Zinc: Essential for cell replication and skin integrity.
- Standard RDA: 11 mg.
- Wound Therapy: 220 mg Zinc Sulfate (providing ~50mg elemental zinc) for 14 days.
Vitamin A: Stimulates the immune response in the wound.
- Standard RDA: 900 mcg RAE.
- Wound Therapy: Often boosted to 10,000 IU short-term if deficiency is suspected.
Arginine & Glutamine:
Amino acids that become "conditionally essential" during trauma to improve blood flow and immune function.
Step 4: Create the Menu (The "Recovery" Plan)
Because John has a low appetite (common after surgery) but high needs, the volume of food must be low, but the density high.
Breakfast: High-Protein Soft Food
- Food: Scrambled Eggs (3 eggs) with cheese.
- Fluid: 1 cup High-Protein Milk (fortified).
- Supplement: Multivitamin + 500mg Vitamin C.
- Why: Eggs provide protein; Vitamin C starts the collagen production early.
Lunch: Collagen Builders
- Food: Chicken Noodle Soup (made with bone broth for extra collagen/protein).
- Add-on: Stir in unflavored protein powder if John can't finish the meat.
- Side: Citrus Salad (Oranges/Grapefruit).
- Why: Bone broth provides amino acids; Citrus provides the Vitamin C vehicle.
Snack: The Therapeutic
- Food: Medical Nutritional Shake (e.g., Ensure Surgery or Boost High Protein).
- Why: It is difficult to eat 120g of protein from solid food when sick. These shakes often contain added Arginine and Zinc specifically for wounds.
Dinner: Zinc Focus
- Food: Braised Beef (very tender) or Dark Meat Turkey.
- Side: Mashed Sweet Potatoes (Vitamin A) + Soft Cooked Carrots.
- Why: Red meat/dark poultry is the best source of Zinc. Beta-carotene from the orange veg supports immune cells.
Step 5: Review Against Standard vs. Medical Need
This table highlights the "Importance" of adjusting DRIs.
| Nutrient | Standard Healthy RDA | John's Medical Need | Consequence of ignoring MNT |
| Calories | ~1,800 (Sedentary) | 2,450 (Healing) | Weight loss, muscle wasting, wound dehiscence. |
| Protein | 64g | 120g | The wound will not close; the immune system fails. |
| Vitamin C | 90mg | 1,000mg | Weak new skin (collagen failure); wound re-opens. |
| Zinc | 11mg | 50mg (Elemental) | Delayed healing; loss of taste/appetite. |
Key Considerations While Creating a Diet Plan Using Dietary Reference Intakes
- Long-Term Goal: Define clear objectives such as weight management, improved energy, disease prevention, or recovery from a medical condition to guide nutrient selection and meal planning.
- Individual Requirements: Consider age, sex, activity level, and health status, as DRIs vary for different populations.
- Nutrient Balance: Ensure the diet provides adequate macronutrients and micronutrients in line with DRI recommendations to support overall health.
- Medical and Lifestyle Factors: Adapt the plan for medical conditions, allergies, dietary restrictions, or lifestyle preferences to ensure safety and adherence.
- Monitoring and Flexibility: Regularly review and adjust the diet plan based on progress, lab results, or changing health needs to maintain effectiveness.
Conclusion
Creating a diet plan using Dietary Reference Intakes DRIs ensures that nutritional needs are met based on age, sex, and health status. By using DRIs as a guide, you can design balanced meals, plan menus, and adjust nutrient intake for specific goals or medical conditions, supporting overall health and well-being.