Weight management consultations today require a thoughtful and structured approach that goes beyond basic dietary advice. As awareness around metabolic health grows, discussions around GLP-1 are becoming an essential part of these consultations.
However, introducing GLP-1 requires careful consideration of timing, individual readiness, and long-term goals.
In this blog, we explore when and how to introduce GLP-1 during weight management consultations, with a focus on informed, balanced, and sustainable decision-making.
What is GLP-1?
GLP-1 is an incretin hormone, a type of metabolic signal released by the endocrine cells (L-cells) of the small intestine and certain neurons in the hindbrain.
Its primary function is to facilitate communication between the digestive system, the pancreas, and the brain to manage the influx of nutrients following a meal.
In its natural state, GLP-1 is highly efficient but short-lived; it is rapidly degraded by an enzyme called DPP-4, usually within minutes of secretion.
How GLP-1 Works?
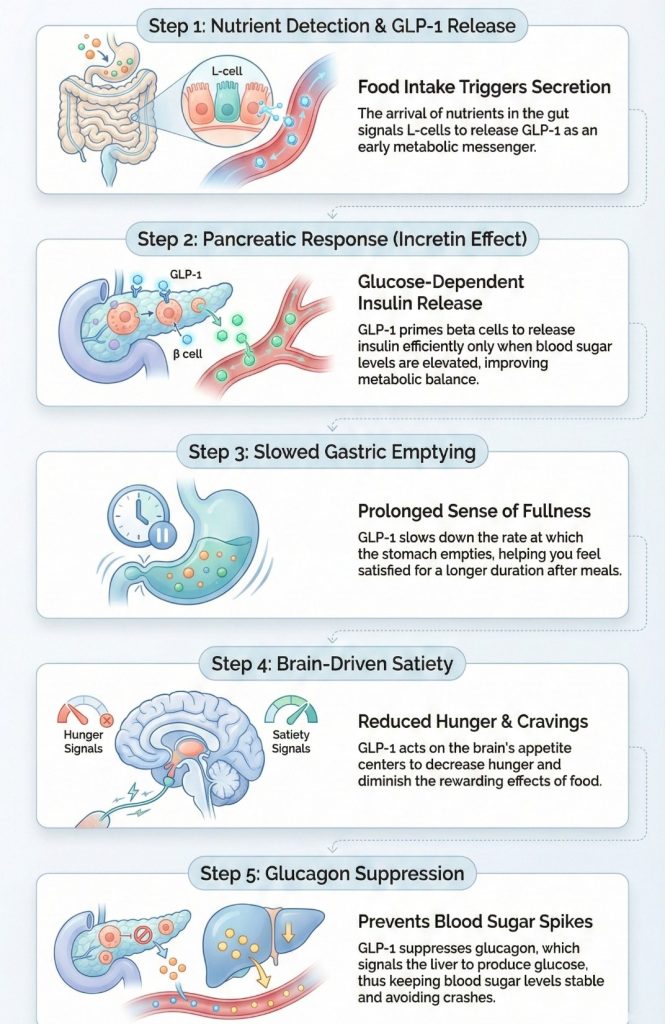
1. Nutrient Detection and Secretion
The process begins the moment you ingest food. As carbohydrates, fats, and proteins enter the small intestine, the L-cells detect their presence. In response, they secrete GLP-1 into the bloodstream. This is the body’s "early warning system" that energy has arrived.
2. The Incretin Effect (Pancreatic Response)
GLP-1 travels to the pancreas, where it binds to specific receptors on beta cells. This triggers a glucose-dependent release of insulin. This is crucial for weight management because it ensures that blood sugar is efficiently transported into cells for energy rather than remaining in the bloodstream or being poorly synthesized.
3. Gastric Emptying Delay (The Fullness)
One of the most significant mechanical roles of GLP-1 is the inhibition of gastric motility. It signals the stomach to slow down the passage of food into the small intestine.
The Result: You feel physically full for a longer duration after eating, which naturally reduces the frequency of food intake.
4. Centrally Mediated Satiety (The Brain Connection)
GLP-1 is capable of crossing the blood-brain barrier or signaling via the vagus nerve to reach the hypothalamus, the brain’s control center.
Suppression of "Food Noise": It downregulates hunger signals and upregulates satiety signals.
Reward Regulation: It impacts the dopaminergic pathways, reducing the "reward" or pleasure derived from high-calorie foods, making it easier to resist cravings.
5. Glucagon Suppression
Simultaneously, GLP-1 prevents the alpha cells of the pancreas from secreting glucagon. Since glucagon tells the liver to release stored sugar into the blood, suppressing it helps keep blood sugar levels stable, preventing the "crashes" that often lead to overeating and weight gain.
To learn more about the complex science behind metabolic health and the effective application of modern therapeutics, the Certificate Program in Nutrition Strategies for Lifelong Health and Wellness offered by Duke University School of Medicine provides a rigorous, evidence-based foundation.
Certificate Program in Nutrition Strategies
Build a strong foundation in whole-food nutrition, metabolic health, and evidence-based dietary strategies to achieve lasting health and wellness transformations.
This 9-week online program covers core areas such as nutrient science, chronic disease management, and GLP-1 therapeutics, enabling practitioners to develop strong weight-loss literacy and distinguish clinically validated advancements from short-lived trends.
Designed by world-class faculty and supported through live mentorship, the program equips learners to apply nutrition and metabolic strategies confidently in real-world clinical and wellness settings.
When to Introduce GLP-1 in a Weight Management Consultation?
1. Clinical Thresholds (The "Hard" Criteria)
Before considering GLP-1 therapy, patients must meet established regulatory criteria. These thresholds serve as the baseline for clinical decision-making:
Obesity: Body Mass Index (BMI) ≥ 30 kg/m²
Overweight with Comorbidity: BMI ≥ 27 kg/m² accompanied by at least one weight-related condition, such as:
- Hypertension
- Dyslipidemia
- Type 2 Diabetes (T2D)
- Obstructive Sleep Apnea (OSA)
Insight: These thresholds are not merely entry requirements but indicators of metabolic risk. The lower threshold (BMI ≥ 27) reflects that adipose tissue can become pathological even before Class I obesity is reached.
2. Metabolic Resistance Point
GLP-1 therapy is most strategically introduced when patients exhibit metabolic adaptations that counteract behavioral interventions:
- Plateau Effect: GLP-1 should be considered when patients adhering to a caloric deficit and exercise program experience a weight plateau, indicating a reduction in Total Daily Energy Expenditure (TDEE) as a physiological defense.
- Aberrant Hunger Signaling ("Food Noise"): Persistent, intrusive thoughts about food despite adequate nutrition indicate neuro-hormonal dysregulation. GLP-1s target hypothalamic satiety centers to modulate this signaling effectively.
3. Failure of Lifestyle Monotherapy
Lifestyle modification (LSM) is foundational but often insufficient for long-term weight maintenance in Class II or III obesity:
- Timing: Patients with a history of weight cycling (“yo-yo dieting”) are unlikely to achieve sustained success through behavioral interventions alone.
- Clinical Logic: In such cases, GLP-1 therapy should be introduced early as an adjunct to LSM rather than a last-resort measure. This approach mitigates metabolic slowdown, improves adherence, and supports sustainable weight loss.
4. Risk Stratification & Contraindications
Patient safety must guide the initiation of GLP-1 therapy, and therapy should be withheld if contraindications are present:
- Absolute Contraindications: Personal or family history of Medullary Thyroid Carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2)
- Cautionary History: Previous pancreatitis or gastroparesis
5. Patient Readiness and Expectations
The successful introduction of GLP-1 depends on patient understanding, psychological readiness, and long-term commitment:
- Mechanism Awareness: Patients must understand that GLP-1 facilitates a caloric deficit and is not a substitute for dietary and lifestyle management.
- Long-Term Perspective: Obesity is a chronic, relapsing condition. GLP-1 therapy is generally a long-term maintenance strategy rather than a short-term solution.
How to Introduce GLP-1?
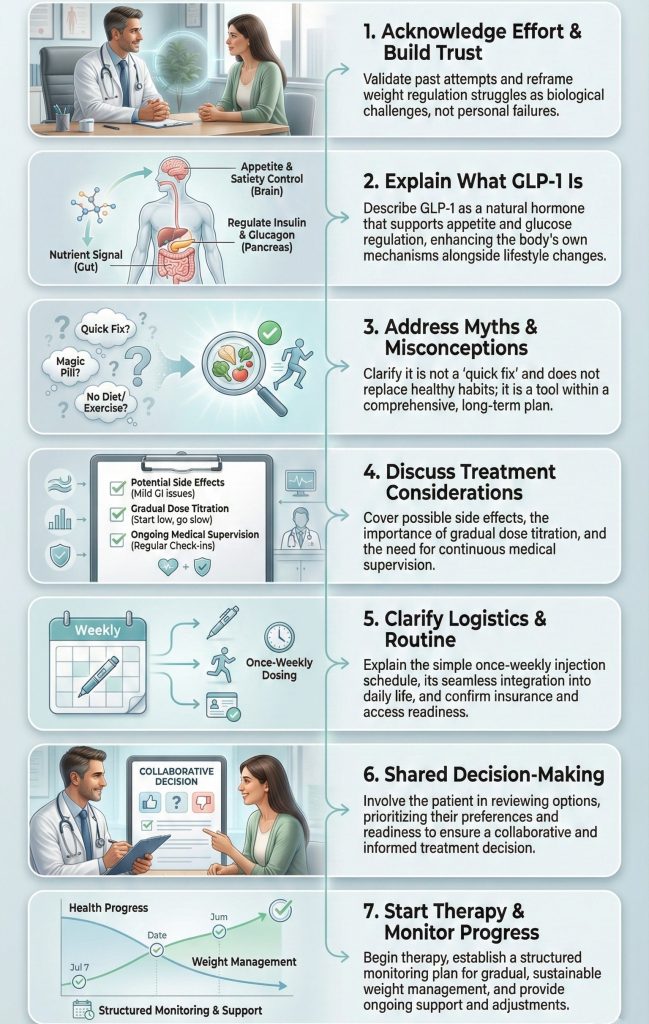
Step 1: Set the Stage and Acknowledge Efforts
Begin by recognizing the patient’s efforts and validating their experiences. This step is about building trust, reducing shame, and helping the patient understand that their challenges are biological, not personal.
Dialogue Example:
- Dr. Chen: "Monica, I see that despite your consistent walks and careful meal planning, your A1c has increased slightly. How have your hunger levels been lately?"
- Monica: "I’m hungry all the time. I eat breakfast, and an hour later I’m already thinking about lunch. I feel like I have no willpower."
- Dr. Chen: "This isn’t a lack of willpower. What you’re experiencing is ‘food noise.’ Your metabolic thermostat is naturally set high, and it’s working against your weight-loss efforts."
Key Insight: Acknowledging effort first helps the patient feel understood and sets a collaborative tone for the consultation.
Step 2: Explain GLP-1 and Its Function
Clearly explain what GLP-1 is and how it works in simple terms. The goal is to help the patient understand that this therapy supports natural physiological processes and works alongside lifestyle changes.
Dialogue Example:
- Dr. Chen: "Have you heard of GLP-1 medications like Ozempic or Wegovy?"
- Monica: "Yes, I’ve seen them on the news. Are they safe?"
- Dr. Chen: "They’ve been used for diabetes for over a decade. GLP-1 works in three main ways:
-Blood Sugar Regulation: Enhances insulin secretion when blood glucose levels rise.
-Satiety Support: Slows gastric emptying, so you feel full longer.
-Appetite Regulation: Sends signals to your brain that your body has enough fuel, helping reduce constant hunger."
Key Insight: Explaining the physiological mechanism helps the patient see GLP-1 as part of a comprehensive, evidence-based plan.
Step 3: Address Myths, Fears, and Common Misconceptions
Explore and clarify any misconceptions or questions the patient may have about GLP-1 therapy. Correct myths about dependency, rapid weight loss, or whether it replaces lifestyle changes. This step ensures the patient has an accurate understanding and sets realistic expectations.
Dialogue Example:
- Dr. Chen: "Some patients wonder if they will have to stay on this medication forever, or if it will replace healthy habits. What have you heard about GLP-1?"
- Monica: "I’ve heard it’s like a quick fix or that I won’t need to watch my diet anymore."
- Dr. Chen: "That’s a common misconception. GLP-1 supports your body’s natural appetite regulation and metabolism, but it works best when combined with consistent lifestyle changes. It’s not a short-term fix, it’s part of a long-term, sustainable plan."
Key Insight: Addressing misconceptions helps patients feel informed, reduces uncertainty, and encourages engagement and adherence.
Step 4: Discuss Treatment Considerations
Clearly and transparently review potential experiences, side effects, and how they will be managed. Preparing the patient for what to expect fosters realistic expectations, builds trust, and encourages adherence to therapy.
Dialogue Example:
- Dr. Chen: "GLP-1 therapy can sometimes cause mild nausea, constipation, diarrhea, or fatigue. Rarely, more serious events like pancreatitis may occur. We reduce risks by starting at a low dose and increasing gradually."
- Monica: "Does the nausea last forever?"
- Dr. Chen: "Usually it’s temporary, mostly in the first few weeks or with dose increases. Gradual titration allows your body to adjust comfortably, and we can provide strategies to manage symptoms if they occur."
Key Insight: Open and honest communication about potential side effects, their duration, and management strategies helps patients feel informed, reassured, and more confident in following the treatment plan.
Step 5: Clarify Logistics and Administration
Explain the practical aspects of therapy, including timing, routine integration, and access. Ensure the patient feels confident about incorporating the treatment into daily life.
Dialogue Example:
- Dr. Chen: "This medication is taken once a week, and it can easily fit into your routine. Just pick a consistent day that works for you. We’ll also make sure your insurance coverage is confirmed, and the medication is available before starting."
- Monica: "That sounds easy. I can plan for one consistent day each week, and knowing everything is ready makes it less stressful."
Key Insight: Focusing on timing, routine, and access rather than the delivery method helps patients feel prepared and confident about adherence.
Step 6: Engage in Shared Decision-Making
Actively involve the patient in the treatment decision. Ensure that the plan reflects their preferences, health goals, and readiness, fostering ownership and commitment. Encourage open dialogue to address concerns, clarify expectations, and confirm understanding.
Dialogue Example:
- Dr. Chen: "Now that we’ve reviewed the therapy, its administration, and follow-up plan, do you feel ready to explore this option?"
- Monica: "Yes, let’s try it. I feel ready if it can help me manage my weight."
Key Insight: Engaging in shared decision-making empowers patients, builds trust, and enhances long-term adherence and satisfaction with the treatment plan.
Step 7: Initiate Therapy with Structured Monitoring
Begin GLP-1 therapy with a clear, structured plan for monitoring progress and adjusting treatment as needed. Emphasize a long-term perspective and gradual, sustainable improvements.
Plan:
- Begin weekly GLP-1 injections with gradual dose escalation to minimize side effects.
- Regularly track weight, appetite, hunger patterns, and relevant metabolic markers such as HbA1c.
- Schedule consistent follow-ups to review progress, adjust doses if necessary, manage side effects, and provide ongoing lifestyle guidance.
- Set realistic expectations for gradual and sustainable weight management outcomes.
Dialogue Example:
- Dr. Chen: "You’ve started the weekly injections, and we’ve been tracking your weight and hunger patterns. How have you been feeling over the past few weeks?"
- Monica: "I feel less hungry between meals, and I’ve noticed some gradual weight loss."
- Dr. Chen: "That’s great progress. We’ll continue monitoring, adjust the dose if needed, and keep supporting your lifestyle habits to ensure these results are sustainable."
- Monica: "I appreciate the guidance; it makes managing my weight feel more achievable."
Key Insight: Combining therapy with structured monitoring and ongoing discussion ensures safe, effective, and sustainable weight management, while keeping the patient engaged, informed, and motivated throughout the process.
This is how you can introduce your patient to GLP-1 therapy, integrating it thoughtfully into a comprehensive weight management plan for safe and sustainable results.
Benefits of GLP-1 in Supporting Effective Weight Management
- Enhanced Adipose Tissue Function
GLP-1 regulates fat storage, reducing visceral fat and promoting the "browning" of white adipose tissue. Brown fat is metabolically active, burning calories to generate heat rather than storing energy.
- Reduction of Hepatic Steatosis
GLP-1 inhibits liver fat production and reduces inflammation, helping clear excess fat from the liver. A healthier liver improves insulin processing and overall metabolism, supporting sustained weight management.
- Cardiovascular and Vascular Benefits
GLP-1 exhibits cardioprotective effects by lowering systemic inflammation and improving endothelial function. Enhanced circulation supports physical activity and increases energy expenditure.
- Hormonal Synergy with Leptin
GLP-1 restores leptin sensitivity, enabling the brain to accurately sense energy stores. This recalibration helps regulate appetite and supports long-term weight control.
- Preservation of Lean Muscle Mass
By stabilizing blood glucose and optimizing insulin sensitivity, GLP-1 promotes the use of glucose and fat for energy efficiently, helping preserve muscle tissue while prioritizing fat loss.
Who Should Not Be Introduced to GLP-1 Immediately?
- Thyroid Cancer Risk: Patients with a personal or family history of Medullary Thyroid Carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
- Pancreatitis History: Patients with a history of pancreatitis, as GLP-1s can increase the risk of recurrence.
- Severe Gastroparesis: Individuals with diagnosed severe stomach paralysis, as these drugs further slow gastric emptying.
- Pregnancy & Breastfeeding: Women who are pregnant, breastfeeding, or planning to conceive in the next 2 months (medication must be stopped beforehand).
- Type 1 Diabetes (Caution): Not FDA-approved for Type 1 (risk of DKA); requires strict specialist supervision if used off-label.
- Active Gallbladder Disease: Patients with active gallstones or gallbladder issues, as rapid weight loss can worsen these conditions.
Conclusion
GLP-1 therapy represents a significant advancement in weight management, offering both metabolic and appetite-regulating benefits.
Its introduction should be guided by a thorough assessment of patient history, lifestyle factors, and clinical goals, alongside structured monitoring to ensure safety and efficacy.
By adopting a personalized and stepwise approach, healthcare providers can optimize outcomes, support sustainable weight loss, and enhance overall patient well-being.
