Healthcare is standing at an inflection point where clinical expertise meets intelligent technology, and the choices made today will shape patient care for decades to come. In this, artificial Intelligence is no longer a pilot confined to innovation labs; it is actively influencing:
- How Diseases Are Detected Earlier
- How Clinicians Make Faster And More Confident Decisions,
- How Health Systems Operate Under Growing Pressure
Yet, the real opportunity lies not just in understanding AI, but in knowing how and when to act on the trends that matter most.
In this blog, we explore the most critical AI trends in healthcare, redefining healthcare, and more importantly, the best practices for implementing AI in healthcare to ensure technology strengthens, rather than replaces, the human core.
The Current State of AI Trends in Healthcare
In 2026, the integration of AI trends in healthcare has progressed from isolated pilot initiatives to a core component of global medical infrastructure.
This shift is driven by substantial capital investment and a strong emphasis on operational efficiency, with the healthcare AI market projected to grow at a CAGR of 43% between 2024 and 2032, reaching an estimated value of $491 billion.
The sector’s rapid evolution is marked by several key financial and operational indicators, such as:
- Generative AI is at the forefront, expanding faster in healthcare than in any other industry and expected to grow at a CAGR of 85% to reach $22 billion by 2027, enabling automation across clinical documentation and drug discovery.
- Early adopters are already demonstrating clear economic value, reporting annual returns of 10–15% over 5-year investment cycles.
- At a system level, AI-driven diagnostics and administrative automation are projected to reduce overall healthcare expenditure by approximately 10%, while simultaneously improving clinical productivity by enabling clinicians to dedicate more time to patient care.
Collectively, these trends position AI as a strategic enabler of sustainable, high-quality healthcare delivery worldwide. To navigate this rapid adoption, professionals must bridge the gap between technical potential and business execution.
The Post Graduate Program in Artificial Intelligence & Machine Learning from Texas McCombs is designed to provide this exact foundation. This comprehensive program covers the full spectrum of AI from supervised and unsupervised learning to Deep Learning and Generative AI.
Post Graduate Program in AI & Machine Learning: Business Applications
Master in-demand AI and machine learning skills with this executive-level AI course—designed to transform professionals into strategic tech leaders.
By mastering these core technologies, healthcare leaders can better interpret market indicators and make informed, strategic decisions that drive AI adoption in their organizations.
Emerging AI Trends In Healthcare
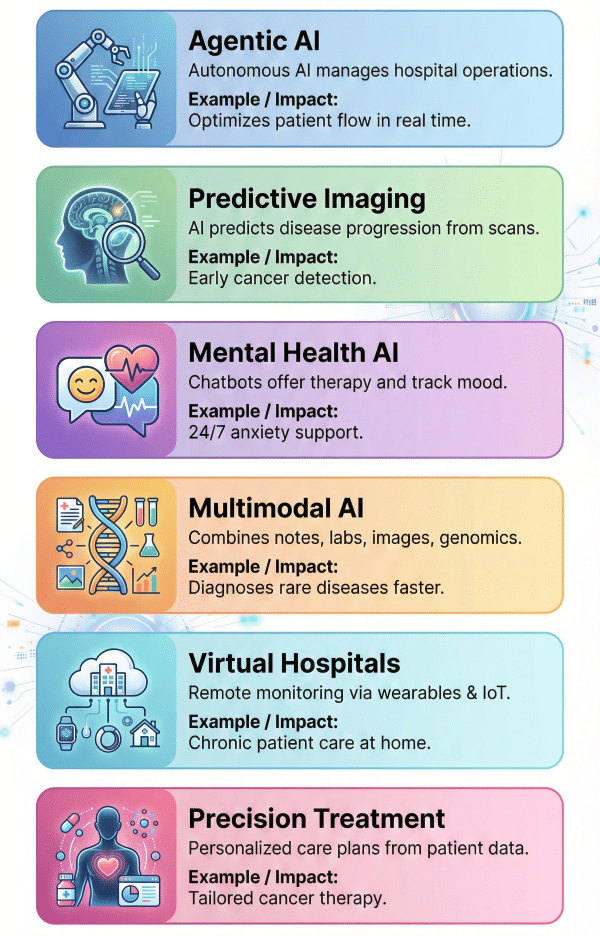
1. Agentic AI for Intelligent Process Automation
We are moving from "passive" AI tools that wait for commands to "agentic" AI that can act independently. Agentic AI refers to systems capable of perceiving their environment, reasoning, and executing complex workflows without constant human oversight.
In a hospital setting, this means AI agents that can coordinate patient schedules, manage supply chains, and even autonomously triage incoming data streams.
How Does It Help?
Example: Managing patient flow in a large tertiary hospital
- Step 1: Continuous Environment Monitoring: The AI agent monitors real-time data from the emergency department, bed management systems, electronic health records, and staffing schedules to maintain a live view of hospital capacity.
- Step 2: Intelligent Risk and Priority Assessment: Based on incoming patient symptoms, vital signs, and historical outcomes, the agent autonomously classifies patients by acuity, for example, identifying high-risk cardiac cases that require immediate admission.
- Step 3: Autonomous Workflow: The AI agent allocates beds, schedules diagnostic tests, and notifies relevant care teams, automatically adjusting plans when delays or emergencies arise.
- Step 4: Operational Coordination & Optimization: If bottlenecks occur, such as delayed discharges or staff shortages, the agent reassigns resources, updates shift plans, and reroutes patients to alternative units to maintain care continuity.
- Step 5: Clinician Oversight & Decision Support: Clinicians receive prioritized dashboards with AI-generated recommendations, enabling them to validate decisions, intervene when necessary, and focus on direct patient care rather than administrative coordination.
2. Predictive Health Assessment & Imaging
Predictive diagnostics utilizes historical data and real-time imaging to foresee health issues before they become critical.
AI algorithms will not just analyze X-rays or MRI scans for current anomalies but will compare them against vast datasets to predict the future progression of diseases like cancer or neurodegenerative disorders.
How Does It Help?
Example: Early detection and intervention in Oncology (Cancer Care)
- Step 1: High-Resolution Data Ingestion: The AI system ingests high-resolution images from CT scans, MRIs, and tissue slides, alongside the patient's genetic profile and family history.
- Step 2: Pattern Recognition and Comparison: The model compares the patient's imaging data against a global dataset of millions of confirmed cancer cases, looking for microscopic irregularities invisible to the human eye.
- Step 3: Predictive Modeling of Disease: Rather than just identifying a tumor, the AI predicts the likelihood of metastasis (spread) and the potential growth rate based on recognized biological patterns.
- Step 4: Risk Stratification and Alert Generation: The system flags "silent" or pre-cancerous markers and generates a risk score, alerting the radiologist to specific regions of interest that require immediate attention.
- Step 5: Treatment Pathway Suggestion: The AI suggests a personalized screening schedule or biopsy plan, allowing doctors to intervene months or years before the disease becomes life-threatening.
3. AI-Driven Mental Health Support
With the rising global demand for mental health services, AI is stepping in to provide accessible, 24/7 support. Advanced Natural Language Processing (NLP) chatbots and therapeutic apps can offer cognitive-behavioral therapy (CBT) techniques, monitor mood patterns, and flag users who may be at risk of a crisis.
How Does It Help?
Example: Providing support to a user with anxiety during off-hours
- Step 1: Conversational Engagement: A user logs into a mental health app late at night, feeling overwhelmed; the AI initiates a conversation using empathetic, non-judgmental language.
- Step 2: Sentiment and Keyword Analysis: The NLP engine analyzes the user's text for specific keywords indicating distress levels, self-harm risks, or specific anxiety triggers.
- Step 3: Therapeutic Technique Application: Based on the analysis, the AI guides the user through evidence-based exercises, such as deep breathing or cognitive reframing (challenging negative thoughts).
- Step 4: Longitudinal Mood Tracking: The AI records the interaction and updates the user's mood chart, identifying patterns or triggers over weeks to share with a human therapist later.
- Step 5: Crisis Intervention Protocols: If the AI detects language indicating immediate danger, it shifts from therapy mode to crisis mode, providing emergency hotline numbers and alerting pre-designated human contacts.
4. Multimodal AI Integration
Future healthcare AI systems will no longer be limited to single data types; they will be multimodal, capable of analyzing and correlating diverse information such as clinical notes, lab results, medical images, and genomic data simultaneously.
By integrating these data streams, multimodal AI provides a holistic view of a patient’s condition, enabling faster, more accurate, and personalized diagnoses.
How Does It Help?
Example: Diagnosing a complex, rare disease with conflicting symptoms
- Step 1: Multi-Source Data Aggregation: The AI system collects patient data from multiple sources: handwritten physician notes, lab reports, genomic sequences, and diagnostic images like X-rays or dermatology photos.
- Step 2: Cross-Modal Correlation: It identifies patterns across these data types linking symptoms described in text to visual indicators in images and genetic predispositions, uncovering connections that may be missed by humans analyzing them separately.
- Step 3: Synthesis and Reasoning: The AI synthesizes all inputs to narrow down possibilities, revealing, for example, that a skin rash aligns with a rare genetic mutation indicated in the DNA report.
- Step 4: Evidence-Based Reporting: A comprehensive diagnostic report is generated, clearly citing the combined evidence from text, imaging, and genetic data that supports the conclusion.
- Step 5: Unified Clinical View: The integrated report allows a multidisciplinary team, such as dermatologists and geneticists, to review findings together and rapidly work on an accurate treatment plan.
5. Virtual Hospitals and Remote Monitoring
Virtual hospitals are transforming healthcare delivery by extending continuous care beyond physical facilities.
Leveraging wearable devices, IoT sensors, and cloud-based platforms, these systems monitor patients’ vital signs, medication adherence, and chronic condition metrics in real time.
This allows healthcare providers to intervene proactively, reduce unnecessary hospital visits, and deliver care to remote or underserved populations.
How Does It Help?
Example: Managing chronic heart failure patients remotely
- Step 1: Continuous Remote Monitoring: Wearable devices track heart rate, blood pressure, oxygen levels, and daily activity, transmitting real-time data to a centralized virtual hospital platform.
- Step 2: Automated Risk Analysis: AI algorithms analyze incoming data trends to detect early signs of deterioration, such as fluid retention or irregular heart rhythms.
- Step 3: Alerts and Intervention: When risks are identified, the system automatically sends alerts to clinicians and patients, prompting timely interventions like medication adjustments or teleconsultations.
- Step 4: Coordinated Care Delivery: The virtual hospital schedules follow-up tests, virtual appointments, and updates care plans based on real-time insights, minimizing the need for physical visits.
- Step 5: Outcome Tracking and Feedback: Patient recovery, adherence, and response to interventions are continuously monitored, enabling care teams to refine treatment protocols and prevent hospital readmissions.
6. Personalized Care and Precision Treatment
Personalized care leverages AI to move beyond one-size-fits-all medicine toward treatments tailored to an individual’s clinical profile, lifestyle, and genetic makeup.
By analyzing longitudinal patient data, including medical history, biomarkers, genomics, and real-world behavior, AI systems can recommend interventions that are optimized for each patient, improving outcomes while reducing unnecessary treatments.
How Does It Help?
Example: Designing a personalized cancer treatment plan
- Step 1: Comprehensive Patient Profiling: The AI system aggregates data from electronic health records, tumor genomics, imaging reports, past treatment responses, and patient lifestyle information.
- Step 2: Predictive Treatment Modeling: Using historical outcomes from similar patient profiles, the AI predicts how the patient is likely to respond to different therapy options, including targeted drugs and immunotherapies.
- Step 3: Risk and Side-Effect Assessment: The system evaluates potential adverse effects based on the patient’s genetics, age, and comorbidities, helping clinicians avoid treatments with high toxicity risk.
- Step 4: Personalized Care Recommendation: AI generates a ranked treatment plan, outlining the most effective therapy, optimal dosage, and expected outcomes, supported by evidence from comparable cases.
- Step 5: Continuous Adaptation and Monitoring: As the patient progresses, real-time data from lab results and follow-up scans are fed back into the model, allowing the treatment plan to be dynamically adjusted for maximum effectiveness.
These emerging AI trends are not just transforming workflows; they’re enabling a new era of predictive, personalized, and efficient healthcare delivery.
Implementing AI Successfully
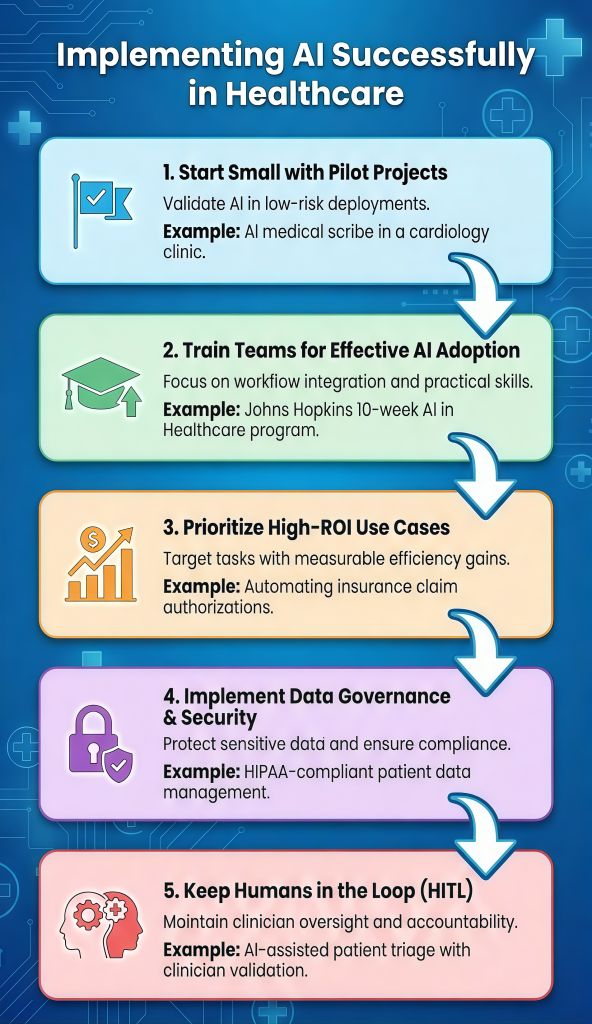
1. Start Small with Pilot Projects
Large-scale digital transformations often fail due to operational complexity. Organizations should instead adopt targeted pilot initiatives, controlled, low-risk deployments designed to validate value before scaling. This approach limits disruption while building stakeholder confidence.
Example: AI Medical Scribe in an Outpatient Clinic
- Focused Deployment: Rather than a hospital-wide rollout, the AI scribe is introduced to a small group of volunteer cardiologists to address a specific issue, excessive clinical documentation time.
- Performance Benchmarking: Key metrics such as documentation time, accuracy, and clinician satisfaction are measured against baseline levels to assess impact objectively.
- Evidence-Based Scaling: Proven outcomes, such as a measurable reduction in documentation time, provide the justification for broader adoption across departments.
2. Train Teams for Effective AI Adoption
Even the most advanced AI algorithms deliver limited value if medical teams cannot use them effectively. Bridging this gap requires a shift from traditional technical training to workflow-focused education, teaching staff not only how the technology functions but how it integrates seamlessly into daily clinical and operational routines.
The Johns Hopkins University AI in Healthcare Certificate Program offers a structured, 10-week curriculum tailored for healthcare and business leaders.
The program emphasizes practical application covering predictive analytics, Large Language Models (LLMs), ethical considerations, and strategies for scaling AI pilots, ensuring teams can translate knowledge into actionable results.
Transform healthcare with AI. Apply now for Johns Hopkins AI in Healthcare Program and enhance patient outcomes with cutting-edge skills
Program Benefits:
- Practical AI Knowledge: Covers predictive analytics, Large Language Models (LLMs), and ethical frameworks, ensuring teams can apply AI in real clinical and operational workflows.
- Healthcare Integration Skills: Introduces the R.O.A.D. Management Framework for implementing AI across care processes.
- Risk & Data Management: Teaches staff to identify project risks, address ethical and regulatory considerations, and manage datasets in Electronic Health Records (EHRs) effectively.
This approach equips clinicians and leaders to confidently validate, adopt, and scale AI solutions, bridging the gap between technology and patient care impact.
3. Prioritize High-ROI Use Case
To secure sustained stakeholder support, early AI initiatives must demonstrate clear return on investment (ROI). ROI should be defined broadly to encompass time savings, error reduction, operational efficiency, and improved patient outcomes. Organizations should focus on high-volume, repetitive tasks that are resource-intensive and susceptible to human error.
Example: Automating Insurance Claim Prior Authorizations
- Bottleneck Identification: High-volume administrative processes, such as manual insurance code verification, are targeted to reduce backlogs and accelerate patient access to care.
- Scalable Automation: AI systems process large volumes of claims in parallel, completing overnight tasks that would otherwise take human teams weeks.
- Value Reinvestment: Quantifiable efficiency gains and cost savings are reinvested into clinical staffing, clearly demonstrating how AI adoption enhances patient care delivery.
4. Implement Data Governance & Security
Healthcare data is highly sensitive and governed by regulations such as HIPAA and GDPR. Effective AI adoption requires a strong governance framework that defines how data is accessed, used, and protected while ensuring compliance and trust.
Example: Securing Patient Data for AI Research
- Data Anonymization & Access Control: Patient data is anonymized or encrypted, with strict role-based access limiting exposure to identifiable information.
- Continuous Compliance Monitoring: Automated audits continuously assess systems against HIPAA, GDPR, and cybersecurity standards.
- Bias & Incident Response: Datasets are routinely tested for bias, and predefined breach-response protocols enable immediate system containment.
5. Keep Humans in the Loop (HITL)
AI systems should augment, not replace human expertise, particularly in high-stakes healthcare decisions. A Human-in-the-Loop (HITL) approach ensures that clinicians and administrators retain oversight, validate AI outputs, and intervene when necessary, preserving accountability, trust, and ethical decision-making.
Example: Clinical Decision Support in Patient Triage
- Decision Validation: AI-generated triage recommendations are reviewed and approved by clinicians before care pathways are finalized.
- Exception Handling: Clinicians can override AI outputs when contextual or patient-specific factors fall outside the model’s assumptions.
- Continuous Learning: Feedback from human decisions is fed back into the system to improve model accuracy, transparency, and reliability over time.
Combining careful planning, robust training, and strong governance, healthcare providers can harness AI to improve operations, support clinicians, and elevate patient care.
Conclusion
AI trends in healthcare are transforming the field, enabling faster diagnoses, personalized treatment, and improved patient outcomes. By staying informed about emerging trends and adopting AI-driven solutions, medical professionals and leaders can drive innovation, enhance efficiency, and shape the future of healthcare.









