Consider a resident physician finishing a grueling 24-hour shift. Fatigued and reviewing patient charts, they still have ten more cases to evaluate, while an intelligent AI-powered assistant has already identified the three highest-risk patients, cross-referenced their symptoms with a global database of rare conditions, and prepared a preliminary treatment plan for review.
This scenario is no longer a distant vision of the future; it demonstrates the real usage of AI in healthcare. For medical leaders, the question has shifted from whether AI will transform patient care to how it can be seamlessly integrated into clinical workflows without compromising the human touch.
In this article, we explore how healthcare organizations can implement AI solutions to enhance patient care, streamline workflows, and support medical professionals in making more informed decisions.
What is AI in the Healthcare Context?
In healthcare, Artificial Intelligence (AI) refers to the use of advanced algorithms and machine learning models to analyze complex medical data, support clinical decision-making, automate administrative tasks, and enhance patient care.
Essentially, AI enables computers and systems to mimic human intelligence, such as reasoning, learning, and problem-solving, allowing them to perform tasks that traditionally required human expertise.
Types of AI applications in healthcare:
1. Diagnostic Support
AI systems, particularly those using Computer Vision and Deep Learning, excel at pattern recognition. In diagnostics, these systems assist clinicians by analyzing medical imagery and lab results with high speed and accuracy, often identifying subtle anomalies that the human eye might miss. For example
- Radiology: AI algorithms analyze X-rays, CT scans, and MRIs to detect abnormalities such as tumors, fractures, or early signs of pneumonia. For example, AI can flag a potential lung nodule for a radiologist to prioritize.
- Pathology: Digital pathology uses AI to scan biopsy slides. It can count cancer cells, grade tumors, and identify specific genetic mutations based on tissue morphology, significantly speeding up diagnosis times.
- Dermatology: Smartphone-based AI applications can analyze images of skin lesions to assess the probability of melanoma or other skin conditions.
2. Predictive Analytics
Predictive analytics shifts healthcare from reactive to proactive. By ingesting vast amounts of historical data and real-time patient metrics (from Electronic Health Records or wearables), AI models can forecast future health events. For examples
- Patient Risk Scoring: AI calculates risk scores for conditions like sepsis or heart failure in real-time. If a patient’s vitals show a trend resembling a pre-septic state, the system alerts the nursing staff hours before the condition becomes critical.
- Disease Progression: For chronic diseases like diabetes or Alzheimer's, AI models analyze longitudinal data to predict how the disease is likely to progress in a specific individual, allowing doctors to intervene early to slow progression.
- Hospital Readmission: Hospitals use predictive models to identify patients with a high likelihood of being readmitted within 30 days, ensuring they receive additional discharge support.
3. Administrative Automation
While less flashy than robotics, administrative AI tackles the massive burden of "busy work" in healthcare. It uses Natural Language Processing (NLP) and Robotic Process Automation (RPA) to streamline operations. For example
- Appointment Scheduling: AI-driven chatbots and booking systems can manage patient schedules, fill cancellations automatically, and send reminders, reducing "no-show" rates.
- Medical Coding & Billing: AI can scan clinical notes and automatically assign the correct medical billing codes (ICD-10). This reduces claim denials caused by human error and speeds up revenue cycles.
- Clinical Documentation: Ambient AI scribes can listen to doctor-patient consultations (with consent) and automatically draft clinical notes, freeing doctors to focus on the patient rather than their screen.
4. Personalized Treatment Recommendations
Also known as Precision Medicine, this application moves away from the "one-size-fits-all" approach. AI integrates genomic data, lifestyle factors, and clinical history to tailor treatments to the individual. For example
- Pharmacogenomics: AI analyzes a patient's genetic makeup to predict how they will metabolize certain drugs. This helps avoid adverse drug reactions and ensures the correct dosage is prescribed from day one.
- Oncology Treatment Plans: AI platforms (like IBM Watson Health in the past) can review thousands of medical journals and clinical trial databases to recommend specific cancer therapies that match the patient's unique tumor mutation profile.
- Mental Health: AI-driven apps can adjust Cognitive Behavioral Therapy (CBT) exercises based on a user's real-time mood and responsiveness to previous sessions.
How to Implement AI in Healthcare?
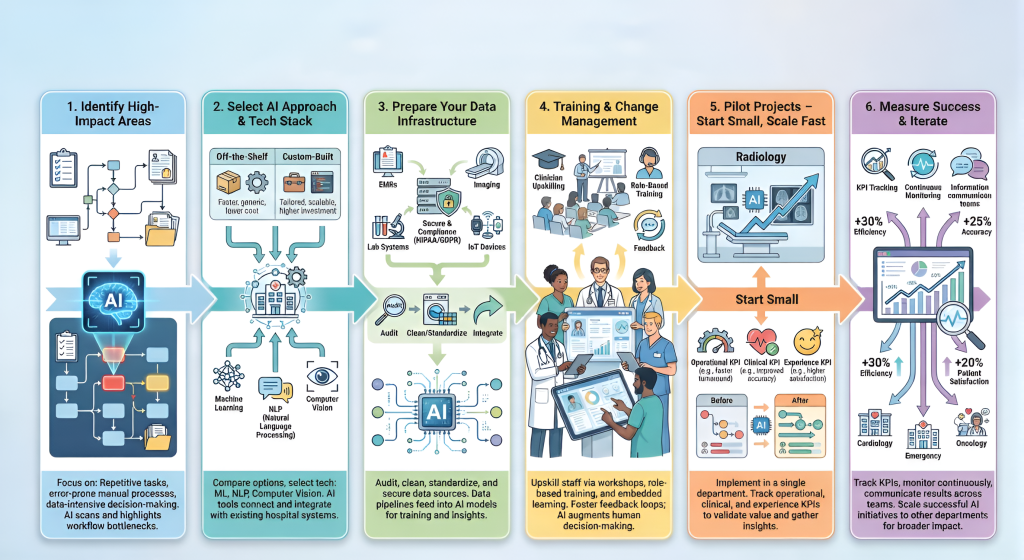
Step 1: Identify High-Impact Areas for AI Implementation
Successful usage of AI in healthcare begins with identifying critical bottleneck areas where human capacity is constrained or where the volume and complexity of data exceed what can be processed efficiently by individuals.
To ensure meaningful outcomes, AI initiatives must be guided by clearly defined objectives rather than technology-driven experimentation.
How to Evaluate Existing Workflows
To identify suitable candidates for AI-driven automation or augmentation, organizations should conduct a structured workflow audit, focusing on processes that exhibit the following characteristics:
- Repetitive, High-Volume Tasks- Processes executed frequently with minimal variation, such as billing codes validation or appointment reminders, are ideal for automation.
- Error-Prone Manual Processes- Tasks that rely heavily on manual data entry and are susceptible to human error due to fatigue or time pressure, such as transferring data between clinical systems.
- Data-Intensive Decision-Making- Situations where clinicians must make decisions within limited timeframes but cannot feasibly analyze large volumes of historical data, for example, reviewing a decade of patient records during a short consultation.
High-Value AI Use Cases in Healthcare
- Clinical Decision Support (CDS)- AI functions as a supplementary layer of clinical oversight by cross-referencing prescriptions with a patient’s complete medical history to identify potential drug interactions, contraindications, or allergies that may otherwise be overlooked.
- Predictive Patient Risk Scoring- Rather than responding after conditions such as sepsis or heart failure worsen, AI continuously analyzes real-time vital signs to generate early warning or deterioration scores, enabling proactive clinical intervention.
- Resource and Workforce Management- Predictive models assess historical admission trends, seasonal illness patterns, and local factors to forecast emergency department demand, allowing hospitals to optimize staffing levels and bed availability while minimizing burnout.
- Patient Engagement and Remote Monitoring- AI-powered virtual assistants manage routine post-discharge follow-ups by monitoring patient responses to standardized health checks. Any indicators of risk automatically trigger escalation to a clinical professional for immediate review.
Step 2: Select the Right AI Approach and Technology Stack
Once you have a problem to solve, you must decide how to solve it. This often comes down to the "Buy vs. Build" decision and selecting the right underlying technology.
Off-the-Shelf vs. Custom-Built Solutions

Once the solution strategy is defined, the next step is selecting the AI technologies that best align with the problem, data type, and clinical environment.
Importantly, each technology brings specific operational and regulatory implications that must be evaluated simultaneously. For example:
- Machine Learning (ML): ML models are well-suited for scenarios where outcomes can be predicted from historical patterns. Examples include patient no-show prediction, early deterioration scoring, and chronic disease risk stratification. These models require large, well-labeled datasets and must be validated for consistency as data volumes grow.
- Natural Language Processing (NLP): NLP enables structured insights from unstructured sources such as physician notes, discharge summaries, and patient feedback. Use cases include EHR documentation automation, data extraction from legacy PDFs, and sentiment analysis.
- Computer Vision: Computer vision systems analyze visual data, such as radiology and dermatology images. Applications include tumor detection, fracture identification, and skin lesion analysis. These systems demand high-quality labeled images, rigorous validation, and compliance with medical device regulations.
Regardless of the AI approach chosen, every solution must be evaluated through a common operational lens, such as:
- Scalability: The system must reliably support growth—from pilot programs to enterprise-wide deployment, without degradation in performance or accuracy.
- Interoperability: AI solutions must integrate seamlessly with existing healthcare systems using standards such as HL7 and FHIR.
- Regulatory and Clinical Validity: Models must be transparent, auditable, and explainable to meet regulatory expectations. Clinical trust depends on avoiding opaque “black-box” decision-making and ensuring validation against real-world data.
These criteria are not secondary checks; they actively shape how data must be collected, stored, governed, and secured. This sets the foundation for Step 3, which is
Step 3: Prepare Your Data Infrastructure
AI outcomes depend directly on the quality and readiness of underlying data. Fragmented, inconsistent, or incomplete datasets reduce accuracy and limit scalability, underscoring the critical role of data preparation in successful AI implementation.
- Audit the Data:
Identify available structured data (databases, spreadsheets) and unstructured data (scanned records, handwritten notes), along with core sources such as EMRs, LIMS, PACS, connected medical devices, and IoT systems. This helps surface gaps, redundancies, and integration requirements.
- Ensure Data Quality and Consistency:
Clean and standardize datasets before model development. Remove duplicates, align clinical terminology and formats (for example, mapping “heart attack” to “myocardial infarction”), and address missing values to improve reliability.
- Integrate Data Across Systems:
AI requires a unified patient view rather than isolated data points. Integrate lab results, imaging, demographic data, and longitudinal clinical history to enable context-aware analysis.
- Secure Data and Ensure Compliance:
Protect sensitive healthcare data through access controls, encryption, and audit trails. Ensure compliance with regulations such as HIPAA and GDPR, and apply de-identification techniques to remove personally identifiable information (PII) from training datasets.
Step 4: Training and Change Management
The primary challenge in healthcare AI adoption is not technology, but organizational culture. Without clinician trust and acceptance, even well-designed AI systems fail to deliver value. Targeted upskilling ensures clinicians remain confident, accountable, and in control of clinical decisions.
For medical professionals and leaders looking to bridge this gap, programs like the Johns Hopkins University Artificial Intelligence in Healthcare Certificate teach AI fundamentals, the R.O.A.D. Management Framework, key machine learning models, ethical considerations, and predictive analytics, equipping participants to evaluate AI solutions, drive innovation, and lead AI adoption in healthcare.
Transform healthcare with AI. Apply now for Johns Hopkins AI in Healthcare Program and enhance patient outcomes with cutting-edge skills
Strategies for Effective Adoption
- Hands-on Workshops and Simulations: Conduct structured training sessions in controlled, sandbox environments where clinicians can interact with AI tools, test edge cases, and understand system behavior without patient risk.
- Clear Positioning of AI as Decision Support: Communicate consistently that AI functions as augmented intelligence, offering recommendations rather than replacing clinical judgment. Reinforce that final decisions always rest with the clinician.
- Role-Based Training Programs: Tailor training to specific user roles, physicians, nurses, administrators, and IT teams, ensuring each group understands how AI supports their responsibilities and decision-making scope.
- Embedded Learning in Clinical Workflows: Integrate short, contextual learning prompts, in-tool guidance, or quick-reference resources within existing systems to reinforce correct usage during day-to-day operations.
- Continuous Feedback and Improvement Loops: Establish formal channels for reporting issues, anomalies, or improvement suggestions. Actively incorporating user feedback into system updates builds trust and long-term adoption.
Step 5: Pilot Projects: Start Small, Scale Fast
Risk management is paramount in healthcare. Never roll out a new AI system across the entire hospital at once.
- Choose a Single Department: Select a department that is eager for innovation or facing a specific bottleneck. Example: Instead of applying predictive scheduling to the whole hospital, start with the Radiology department to optimize MRI machine usage.
- Define Measurable KPIs: You need concrete proof that the pilot worked before you can ask for more budget.
-Operational KPIs: Reduced patient wait times, lower appointment cancellation rates.
-Clinical KPIs: Diagnosis speed (time-to-treatment), reduction in false positives.
-Experience KPIs: Staff satisfaction scores (reduction in after-hours charting).
- Gather and Refine: Collect qualitative feedback. Does the AI integrate smoothly into the UI, or does it require five extra clicks? Use this "beta" phase to smooth out workflow friction before the wider launch.
Step 6: Measure Success and Iterate
Building on insights from pilot projects (Step 5), the next step is to systematically evaluate outcomes, refine models, and expand successful AI initiatives.
- Track Defined KPIs:
Measure performance against the metrics established during the pilot, such as error reduction, diagnostic speed, workflow efficiency, and patient satisfaction. Example: Monitor whether AI-assisted radiology reporting reduces turnaround time from 24 hours to under 6 hours and lowers reporting errors by 25%.
- Continuously Monitor and Update Models:
Regularly review AI outputs to identify errors or drift, retrain models as necessary to maintain accuracy and reliability. Example: Adjust predictive patient risk scoring models in the ICU to maintain a 90%+ accuracy rate in identifying high-risk patients.
- Communicate Results Across Teams:
Share outcomes with clinicians, operational staff, and leadership to reinforce trust, adoption, and engagement. Example: Present improvements such as a 15% increase in patient satisfaction scores or a 20% reduction in missed appointments at departmental meetings.
- Scale Successful Initiatives:
Expand AI deployment to additional departments or processes based on pilot success and validated performance. Example: After radiology success, roll out AI-driven workflow automation in pathology or cardiology, aiming for similar reductions in turnaround time and error rates.
Following these steps ensures a structured, measurable, and scalable approach to AI adoption in healthcare, maximizing both clinical impact and operational efficiency.
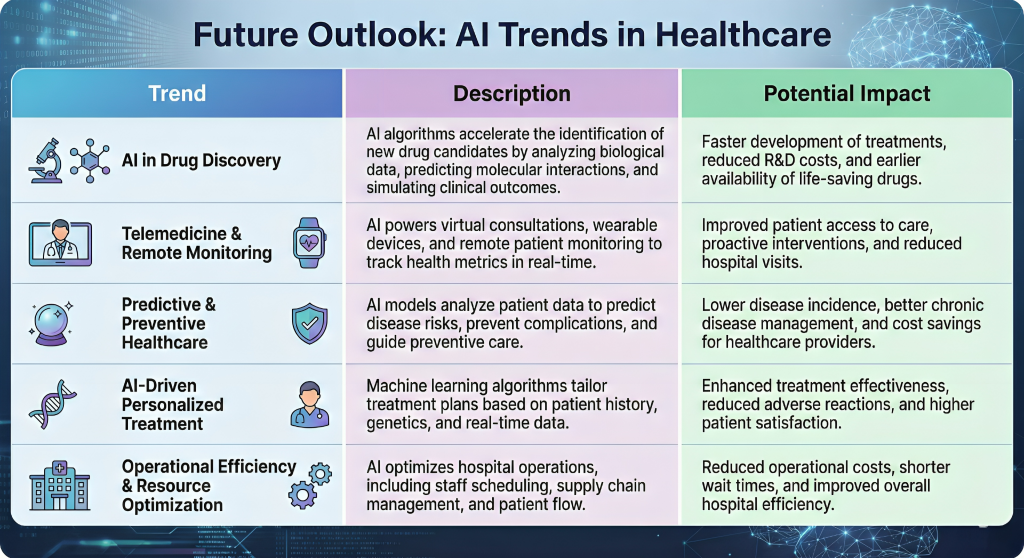
Future Outlook
Conclusion
Implementing AI in healthcare is no longer a futuristic concept; it’s a practical strategy to improve patient care, streamline operations, and drive innovation.
By identifying high-impact areas, preparing quality data, choosing the right AI solutions, and starting with pilot projects, healthcare organizations can confidently embark on their AI journey.
With careful planning, ethical practices, and continuous learning, AI can become a powerful ally in delivering smarter, faster, and more personalized healthcare.









